Strokes and Cerebral Haemodynamics
Strokes are the second leading cause of death in Spain, and the most frequent cause of disability in adults around the world. Every two seconds, someone suffers a stroke and it is estimated that one in six people will suffer one in their lifetime. In fact, it is one of the pathologies that requires the longest hospital stay and the second most common cause of dementia.
The Stroke and Cerebral Haemodynamics Unit provides excellent comprehensive care to patients who have had a cerebral infarction. The main aspects of the Unit’s activity are: to promote innovation, continuous improvement of quality care, teaching, research and clinical management.
Description
Our mission at the Stroke and Cerebral Haemodynamics Unit is to achieve the highest quality healthcare standards through defined quality objectives. We aspire to make our unit a centre for clinical management providing comprehensive, multidisciplinary care for strokes in the acute phase, focused on achieving a high level of excellence as a level three centre for the resolution of the most complex cases of neurovascular pathology.
Members of the Stroke Unit share the values of commitment, teamwork, innovation and vocation to serve, all to help achieve the following strategic objectives:
- To reduce the time between the onset of symptoms and effective cerebral reperfusion (restoration of the blood flow to the brain).
- To increase the number of reperfusion treatments to 25% (currently 14%).
- To reduce the adjusted average stay to the risk by optimising triage and referring patients by telemedicine.
- To ensure early multidisciplinary assessment of intracranial haemorrhages.
- To consolidate leadership of the Unit in procedures for vascular neuro-interventionism.
- To integrate early rehabilitation protocols in stroke patients.
- To offer a comprehensive training programme for stroke nursing.
- To promote a cross-cutting approach to transfer knowledge among the professionals involved.
- To apply and evaluate the Unit’s Quality and Sustainability Plan.
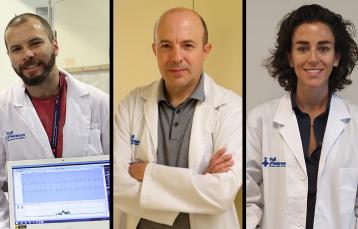
Our multi-disciplinary team is made up of eight vascular neurologists, three neuro-interventionists, two stroke nurses per shift, rehabilitators and nursing assistants. We work closely with professionals from other specialties such as neuroradiology, cardiology, neurosurgery and rehabilitation. This means that in 80% of cases, only 12 hours pass between the arrival of patients and admission to the Unit , which allows patients to be diagnosed in 48 hours in 80% of cases, reducing the average stay to under 2.9 days, despite receiving highly complex cases.
Pioneers in innovation
The progress we have made in recent years has secured our position as leaders both locally and nationally, thanks to the development of innovative and effective treatments that reduce the social and economic burden of strokes in our society. This allows us to be pioneers:
- We offer nine beds with continuous haemodynamic monitoring systems that allow us to monitor, minute by minute, the evolution of patients together with a telemedicine service, watching the condition of the patient 24 hours a day. In addition, two of these beds are for monitoring cerebral and clinical haemodynamics for transient ischemic attacks, meaning we can assess and diagnose patients in less than 24 hours; this is backed up by constant availability on our emergency ward.
- We were the first centre to instate Code Stroke in 1998, as well as pioneering the implementation of the neurovascular systematic diagnosis using Doppler ultrasound, which applies ultrasound to detect blood flow, in our Emergency room. Thus, we are proud to have contributed significantly to the development of treatment strategies such as sonothrombolysis, and we have received international recognition for our leadership in multicentre clinical studies.
- We have integrated vascular neurointerventions into the structure of the Unit. This functional model means we can substantially reduce time needed for brain reperfusion and optimise patient care and management of treatment, while maintaining the quality standards of the Stroke Unit in the neuro-intervention room.
- We have installed a Doppler ultrasound station, an echocardiograph and a vascular neuro-interventionism room, all made available to the medical team working there.
- We also have a gym for early rehabilitation. The facilities, located on the second floor of the General Hospital, cover some 294 m2.
Technology for improving health
Technology is a tool to help improve the health and quality of life of our patients. A good example of this is the mobile apps we work with, such as Farmalarm, an instrument for patients who have returned home after suffering a stroke and which allows them to receive continuous, personalised monitoring to make sure they comply with their treatment plans and controlling vascular risk factors.
We also have the Teleictus Mòbil system to assess and follow up on patients via videoconference before they arrive at the Hospital, and we use telemedicine to perform non-invasive neurovascular scans for 24 hours, offering high-quality urgent care for strokes, not just in our referral area, but also in other centres that do not have on-call neurologists.
Portfolio of services
Urgent neurological clinical assessment, available 24 hours a day 7 days a week (24/7).
- Code Stroke available in and out-of-hospital 24/7.
- Continuous video monitoring of acute strokes, hospitalisation in the Stroke Unit and Vascular Neuro-interventionism, available 24/7.
- Urgent multimodal systemic haemodynamic monitoring, 24/7.
- Doppler ultrasound of supra-aortic patients, 24/7.
- Transcranial Doppler ultrasound, 24/7.
- Prehospital sonogram diagnosis (ambulances) of ischemic and haemorrhagic stroke.
- Continuous and real-time monitoring of arterial recanalisations, 24/7.
- Continuous outpatient monitoring of blood pressure.
- Urgent cardiac ultrasound in patients with acute stroke.
- Telemedicine: neurological assessment, evaluation and treatment of reperfusion in provincial hospitals.
- Treatment of systemic reperfusion (endovenous thrombolysis).
- Vascular neuro-interventionism.
- Identification, diagnosis and selection of patients with candidates for decompressing hemicraniectomy.
- Clinical trials of treatments and experimental procedures in the acute stroke phase.
- Continuous outpatient monitoring of cardiac arrhythmia.