Asthma is one of the leading respiratory diseases worldwide and since SARS-CoV-2 is a respiratory pathogen, it is important to quantify the risk that the current COVID-19 pandemic may represent for asthma patients. A team of researchers from the Pneumology group at the Vall d'Hebron Research Institute (VHIR) have carried out a study to answer two questions: Is asthma a risk factor for COVID-19 or, on the contrary, would protect against the disease? Are phenotypes important? On the one hand, they have found that asthma does not seem to be related to a worse evolution of COVID-19 and, on the other, the importance of phenotypes has been highlighted since asthma could be a protective factor against SARS-CoV-2 virus infection, especially in asthmatic patients with T2 phenotype. The study is published in the ERJ Open Research.
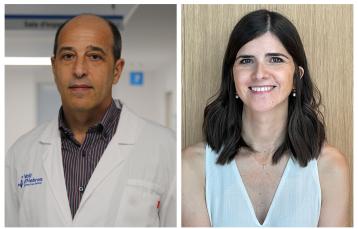
To solve these two questions, the researchers, led by Doctors María Jesús Cruz, head of the VHIR Pneumology research group and Xavier Muñoz, principal investigator of the same group and members of the CIBER Respiratory Diseases (CIBERES) carried out a study with 71 asthmatic patients who were admitted to the Vall d'Hebron University Hospital with SARS-CoV-2 pneumonia from March 1 to June 30.
The project hypothesis was based on the first studies published in China, Korea and New York on the relationship between SARS-CoV-2 and patients with bronchial asthma in whom asthma was not identified as a risk factor for developing severe COVID -19. Based on this information, the objective of the study was to estimate the prevalence of asthma in hospitalized patients with severe coronavirus pneumonia, in a geographic region where the prevalence of asthma is around 6%.
In the study, a cross-sectional analysis was performed of all patients admitted to Vall d'Hebron with SARS-CoV-2 infection confirmed by PCR (2,226 patients). From the electronic medical record, data such as age, sex, whether or not they suffered from asthma, and the presence of comorbidities were recorded. In the 71 patients with asthma, data were collected on the phenotype, severity, and the treatment for asthma. The severity of COVID-19 was recorded based on the needs for oxygen and ventilation support and the findings of the chest X-ray.
According to the phenotype, asthmatic patients were divided into two groups: T2 (with subgroups T2-Th2 and T2-ILC2) and Non-T2. The patients were considered to have a T2-Th2 phenotype if, according to the medical history, they were allergic; and a T2-ILC2 phenotype if they were not allergic but the absolute eosinophil count in peripheral blood was greater than 300 cells per cubic millimetre. In the case of patients with elevated IgE and a positive puncture test or specific IgE to some of the usual pneumoallergens, they were considered allergic. Patients who did not meet any of these criteria were classified as a Non-T2 phenotype. 76% of these patients had some comorbidity (previous disease) in addition to asthma.
Of these 71 patients, 42 had the Non-T2 phenotype, while 20 were allergic (T2-Th2) and 9 were eosinophilic (T2-ILC2). In patients with the Non-T2 phenotype, a greater severity of COVID-19 was observed. However, evolution with standard treatment was good in 67 (94%) patients, while four died.
Among patients receiving inhaled corticosteroid treatment for asthma, no correlation was observed between inhaled corticosteroid dose and COVID-19 severity.
"Our results support the idea that asthma does not appear to be a risk factor for the development of COVID-19, at least in hospitalized patients with more serious forms of infection", explains Xavier Muñoz. Therefore, the question arises whether it could be a protective factor.
In the present study, we found that only 3.2% of hospitalized patients with severe disease had asthma, a lower prevalence than that of the general population in our geographic area, which is around 6%. "If we also take into account that 54 (76%) of the 71 affected patients had comorbidities that have been shown to be directly related to the involvement of SARS-CoV-2, the prevalence of asthmatics without other disorders suffering from severe disease is reduced to only 0.8%, a similar rate to that reported by 0.9% by LI et al in Wuhan, where the prevalence of asthma is also 6%", reflects María Jesús Cruz.
The explanation for this finding is unclear. Although some authors have suggested that treatment with inhaled corticosteroids can protect these patients from the disease by decreasing the production of cytosines; others believe that it would be the presence of activated eosinophils that would protect individuals from infection, in a similar way to what has already been described for other viruses. And there is a third hypothesis that points to the interrelation between asthma and the renin-angiotensin system: it is already known that the activation of the ACE2 receptor is the gateway of the virus to cells and also regulates the asthma response in an animal model of asthma. Therefore, it could be speculated that the reduced activity of this receptor, that favours the development of asthma, could also prevent the expression of the virus.
"However, in the present study we did not find a relationship between the dose of inhaled corticosteroids and the severity of COVID-19, nor has a relationship been found between the level of eosinophils and the possible protection against the virus, nor has it been seen that exacerbate asthma as it happens with other coronaviruses", points out Xavier Muñoz.
"Although the present study has inherent limitations due to its design, the results suggest that asthma could be a protective factor against SARS-CoV-2 virus infection, especially in asthmatic patients with the T2 phenotype. If they are reproduced in studies with a larger number of patients, they can open a new avenue of research in the fight against SARS-CoV-2", concludes Xavier Muñoz.